As healthcare systems continue to scale in complexity, documentation has become one of the largest hidden drivers of clinician burnout. In 2026, physicians spend an average of two additional hours per day on clinical documentation, much of it outside scheduled patient hours. AI medical scribes have moved from experimental tools to core infrastructure, helping reduce after-hours charting, improve note quality, and restore time for direct patient care.
Modern medical scribe platforms use advanced natural language processing, clinical context modeling, and real-time speech recognition to generate structured medical records during or immediately after patient encounters. These systems capture conversations, extract relevant clinical details, and format notes to align with specialty-specific and organizational standards. To operate safely in clinical environments, leading solutions now rely on enterprise-grade encryption, strict access controls, and configurable workflows that adapt to individual physician preferences.
AI medical scribes significantly reduce administrative workload, improve documentation consistency, and support better physician patient interactions. Recent performance benchmarks show that AI-based systems now match or exceed human transcription accuracy in most outpatient and specialty settings, particularly in environments with standardized workflows and clear clinical protocols.
When evaluating medical scribe solutions, healthcare organizations should focus on a few critical factors:
Accuracy in recognizing complex medical terminology
Demonstrated time savings and return on investment
Strong data security and regulatory compliance
Seamless compatibility with existing EHR and EMR systems
This technology is reshaping how clinical documentation is produced and consumed. While the market is crowded, a smaller set of platforms consistently delivers reliable performance, clinical accuracy, and operational value. Below is a curated review of seven AI medical scribe solutions that stand out across these criteria.
1. Twofold
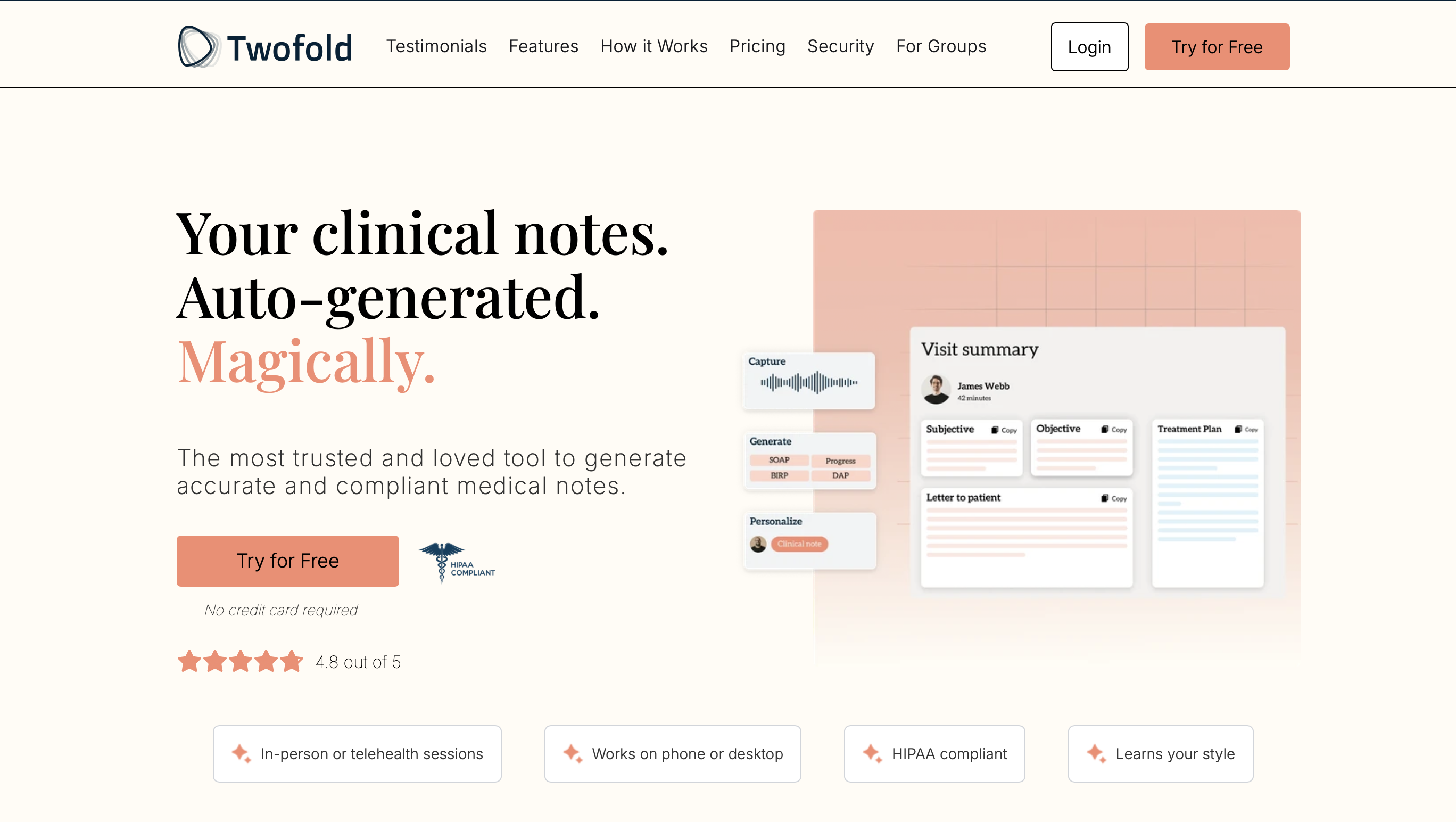
Twofold developed a dedicated AI medical scribe designed for clinicians who want to generate accurate and compliant medical notes with ease. It helps focus on patient care while eliminating the need for excessive paperwork.
It offers 99% transcription accuracy and learns each user’s unique writing style to generate notes that feel natural. Key features include AI-assisted CPT/ICD-10 coding, customizable templates for over 25 specialties, and seamless integration with major EHR/EMR systems.
Some features about Twofold:
-
HIPAA and HITECH compliant, it never stores data to train its models.
-
Let physicians copy and paste their notes into EHR or EMR.
-
Can learn the physician's unique writing style over time
-
Can capture virtual and office conversations for up to 1.5 hours
Twofold lets you record conversions and generate personalized notes and patient instructions. The notes can be reviewed and edited before being sent to the EHR. Even if you don't want to capture the conversation, you can send a quick recap of the consultations to the tool and have it auto-generate detailed notes.
Since Twofold doesn’t store any audio or data, the recordings are processed in real time. So, as soon as the notes are generated, the data is deleted.
Twofold's free trial option is an excellent opportunity to test the tool. Pricing starts from a free plan (20 notes/month) to $49/month for unlimited notes. It's an ideal option for healthcare providers, mental health professionals, and therapy practices aiming to reduce administrative burden with a simple and accurate tool.
2. PatientNotes
PatientNotes helps allied health, general medicine, and specialist professionals generate AI-powered clinical notes, treatment plans, referral letters, and medicolegal reports. It converts voices into rich, detailed medical notes and saves healthcare providers time by relying on AI while still ensuring compliance with privacy and security regulations.
The platform integrates with major Medical Practice Management Systems and telehealth platforms, ensuring flexible use across devices. PatientNotes is HIPAA-compliant and emphasizes workflow efficiency and secure data handling.
Some more features include:
-
Voice-to-text to record patient consultations and clinicians' dictations
-
Customized settings to generate clinical notes in a personalized way
-
Reduces time needed on admin tasks like client action plans, medical letters, and reports
-
iOS app lets healthcare professionals dictate notes and capture sessions on iPhone and iPad
PatientNotes lets you create notes that comply with the industry standards and protocols you choose. There's a Prompt Library to select from plug-and-play letter templates. However, Healthcare providers can even upload their own letter templates to maintain their organizational standards.
Healthcare professionals can try PatientNote's 14-day free trial, watch a 15-minute free demo, or request a discovery call to learn about its best features before subscribing. This digital scribe is an ideal choice for medical practices and telehealth providers aiming to reduce paperwork and improve documentation accuracy without disrupting care.
3. Revmaxx
RevMaxx is an AI medical scribe for specialized healthcare providers, such as cardiologists, dentists, and emergency departments. They claim to generate 95% accurate notes. RevMaxx focuses on adapting to the specialties of healthcare professionals. They offer a variety of templates and settings to accommodate different documentation styles.
It features automated ICD-10, HCC & CPT coding, seamless copy-paste to EHR, and SOAP Note Customization, and apart from these, key features include:
-
Built-in automated coding to reduce errors and ensure accurate records
-
EHR Agnostic System allows seamless EHR integration without any technical setup
-
RAF Score Calculator to instantly calculate expected healthcare costs for patients
RevMaxx employs advanced NLP to convert doctor-patient conversations into structured, standardized medical notes automatically. It integrates with popular hospital systems like Epic and Cerner, allowing easy adoption without workflow disruption.
Apart from note-taking, RevMaxx promises accuracy for a variety of medical specialties. Healthcare providers can try the demo or opt for the free trial to explore the innovative features of RevMaxx.
4. DeepScribe
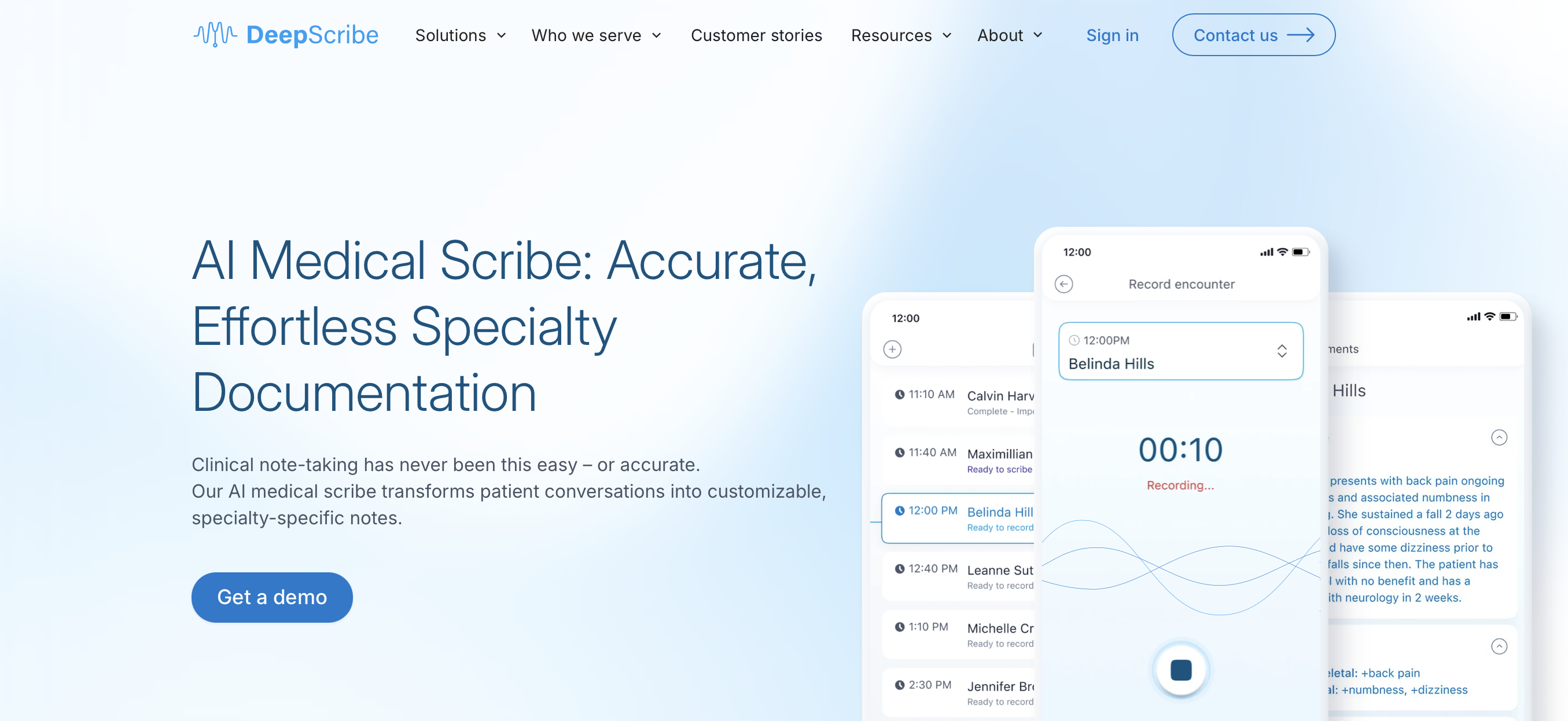
DeepScribe creates context-aware, specialty-specific, and customized patient notes from consultations. This tool offers documentation for health systems, private practices, and specialty care, including oncology, cardiology, and orthopedics. The KLAS Spotlight Report has rated DeepScribe 98.8 out of 100 in the AI technology category.
DeepScribe’s features include:
-
Can create context-aware notes from past and current patient data
-
Compatible with face-to-face and telehealth visits
-
Can be used to record and process 25+ languages, supporting diverse cultural backgrounds
-
Uses ICD-10 codes to simplify billing and coding from patient conversations
-
HIPAA Compliant and end-to-end data encryption prevents data misuse
-
Multi-factor authentication and limited user access allow only authorized persons to access the platform
DeepScribe is not limited to note generation only. It also allows billing and coding from patient conversations. The physicians can earn from both fee-for-service and value-based care. DeepScribe even shares key patient data before, during, and after patient visits to help make the best clinical decisions.
To use DeepScribe, healthcare providers need to submit a request with their details and request a demo from the DeepScribe team. It's an ideal option for providers who want to create value-based care programs and context-aware insights.
5. Microsoft Dragon Copilot (Formerly Nuance DAX)

Microsoft Dragon Copilot helps improve clinician well-being while enhancing the quality of patient care. With Microsoft Dragon Copilot, healthcare professionals can create customized documents, including encounter summaries, evidence summaries, reference letters, and after-visit summaries. This tool is dedicated to providing AI that is trustworthy, secure, safe, and private for all.
Microsoft Dragon Copilot’s features include:
-
Supports multiple devices and users, including mobile, web, desktop, and embedded in EHRs
-
Can be used with a translator to receive English documentation from any language
-
Documents can be customized across a wide range of care settings
-
Identifies up to 12 types of order or patient-followup content from conversations, such as medications or procedures
Dragon Copilot is ideal for healthcare professionals looking to automate administrative tasks with responsible AI in a secure and protected cloud. You can watch the demo on Dragon Copilot's webpage to get started.
6. Suki

Suki acts as a digital assistant for clinicians, automatically generating documentation, orders, ICD-10 and HCC coding for accurate billing, and answering questions. It uses voice-enabled dictation and natural language processing to automate clinical documentation. The real-time data is directly incorporated into most EHRs, with no copy-pasting or complex steps required.
Key features include:
-
Accessible from iOS, Android, desktop, and web
-
SOC2 Type 2 certified and HIPAA compliant
-
Can be scaled with the largest health systems
-
Can pull precharted and live data from EHR to generate high-quality notes and insights
Suki is designed for clinicians in all settings, including ambulatory, inpatient, telehealth, and home health. Healthcare providers should opt for Suki for its voice-driven multi-task handling and question-answering capabilities across all devices.
Suki’s pricing starts at $399 per month, and to get started with Suki, submit your information to contact Suki's sales team.
7. ScribeAmerica AI
ScribeAmerica’s Speke is the AI-powered medical scribe whose language models are fine-tuned by 20+ years of scribing excellence. Speke is designed for all types of healthcare settings, including urgent care, specialized medicine, veterinary care, and family medicine.
ScribeAmerica’s features include:
-
White-glove implementation support ensures that training and ongoing support are taken care of by real experts
-
HIPAA Compliant, SOC2 Type 2 Certified for added privacy and security
-
Offer real-time listing, custom note generation, and direct EHR entry
ScribeAmerica is for healthcare professionals seeking the latest AI-backed scribing technology, along with initial and ongoing support from a seasoned team. Contact the ScribeAmerica team to get started.
Conclusion
A common concern among clinicians is whether AI medical scribes can truly understand clinical nuance and medical context. In 2026, the answer is increasingly clear. With advances in large language models trained on clinical data, modern scribe platforms are capable of producing accurate, structured, and context-aware documentation at scale.
Leading AI medical scribes are now trusted to handle complex terminology, specialty-specific workflows, and evolving care models. When implemented correctly, they deliver measurable improvements across clinical operations.
-
In practice, AI medical scribes help organizations:
-
Reduce administrative workload for clinicians
-
Decrease burnout and improve work life balance
-
Increase patient facing time without extending workdays
-
Improve documentation quality and patient satisfaction
The most successful deployments are not driven by features alone. They are driven by fit. Choose platforms that integrate cleanly with existing workflows, align with your clinical setting, and offer responsive onboarding and support. When AI scribing complements how clinicians already work, it becomes a durable advantage rather than another system to manage.


